Cardiac System
Abnormal Physical Examination Findings
| Finding | Conditions |
|---|---|
| Kussmaul sign | Cardiac tamponade Right heart failure Restrictive cardiomyopathy |
| Pulsus paradoxus | Cardiac tamponade Obstructive lung diseases |
| Pulsus parvus et tardus | Aortic stenosis |
| Pulsus alternans | LV systolic dysfunction |
| Differential cyanosis | Eisenmenger syndrome of PDA |
| Reverse differential cyanosis | Transposition of great artery (TGA) |
Abnormal Heart Sounds
Extra Heart Sounds
| Heart Sound | Synonym | Mechanism | Diseases |
|---|---|---|---|
| S2 | Opening snap | MV & TV opening | MS & TS |
| S3 | Ventricular gallop | Ventricular filling Volume overload | HF & DCMP & MR & TR |
| S4 | Atrial gallop | Atrial contraction Diastolic dysfunction | HF & HCMP |
Abnormal Splitting
| Type | Etiology |
|---|---|
| Wide | Pulmonary stenosis RBBB |
| Paradoxical | Aortic stenosis LBBB |
| Fixed | ASD |
Murmurs
| Disease | Phase | ↑ Preload | ↑ Afterload |
|---|---|---|---|
| VSD | Systolic | ↑ | ↑ |
| AS | Systolic | ↑ | ↓ |
| AR | Diastolic | ↑ | ↑ |
| MS | Diastolic | ↑ | - |
| MR | Systolic | ↑ | ↑ |
| MVP | Systolic | ↓ | ↓ |
| HCMP | Systolic | ↓ | ↓ |
Grading of Murmurs
| Grade | Thrill | Stethoscope |
|---|---|---|
| 1 | - | Against |
| 2 | - | Against |
| 3 | - | Against |
| 4 | + | Against |
| 5 | + | Partially off |
| 6 | + | Completely off |
Abnormal ECG Findings
| Finding | Conditions |
|---|---|
| Diffuse ST elevation | Acute pericarditis |
| Electrical alternans | Pericardial effusion |
| Low voltage | Pericardial effusion |
| Widened QRS | Ventricular rhythm Hyperkalemia TCA toxicity |
| Bidirectional VT | Digitalis toxicity |
| S1Q3T3 | Pulmonary embolism |
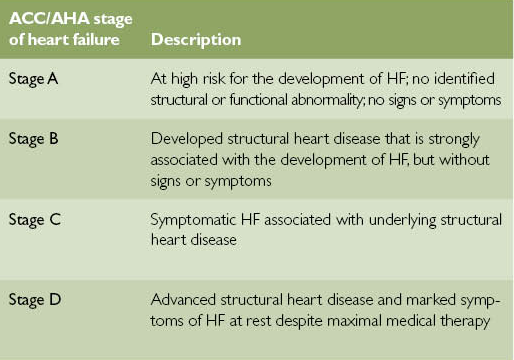
| Delta waves | Wolff-Parkinson-White (WPW) syndrome |
| U waves | Hypokalemia |
| Sine waves | Hyperkalemia |
| Osborn waves | Hypothermia |
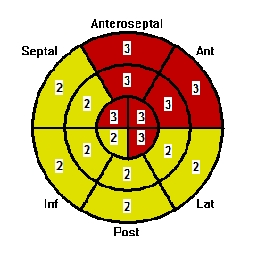
Regional Wall Motion Abnormality
Inotropes
| Mechanism | Medication |
|---|---|
| Na-K pump blockers | Digitalis |
| β1 agonists | Norepinephrine Epinephrine Isoproterenol Dobutamine Dopamine |
| PDE inhibitors | Inamrinone Milrinone |
Effects of Inotropes
| Inotrope | Mechanism | CO | SVR | MAP | IE |
|---|---|---|---|---|---|
| Norepinephrine | α1 > β1 | - | ↑ (1°) | ↑ | 100 |
| Epinephrine | β1 > β2 > α1 | ↑ (1°) | ↓ | ↑ | 100 |
| Isoproterenol | β1 = β2 | ↑ (1°) | ↓ (1°) | - | 100 |
| Dobutamine | β1 > β2 | ↑ (1°) | ↓ | ↑ | 1 |
| Dopamine | D > β1 > α1 | ↑ | ↓ (1°) | ↓ | 1 |
| Inamrinone Milrinone | - | ↑ (1°) | - | ↑ | 15 |
- Cardiac output (CO)
- Systemic vascular resistance (SVR)
- Mean arterial pressure (MAP)
- Inotropic equivalent (IE)
Inotropic Equivalent (IE)
| Parameter | Σ(E × R) |
|---|---|
| E | Equivalent |
| R | Rate (µg/kg/min) |
Medications Slowing Conduction {ABCD}
- Adenosine
- Amiodarone
- β antagonists
- Ca channel blockers
- Digitalis
Atrial Septal Defects (ASD)
| Type | Prevalence |
|---|---|
| Secundum | 70% |
| Primum | 20% |
| Sinus venosus | 10% |
| Coronary sinus | < 1% |
.jpg)
Ventricular Septal Defects (VSD)
.png)
Cyanotic Congenital Heart Defects (CHD) {5T-HE}
| Defect | Obligatory Shunt | Cyanosis |
|---|---|---|
| Truncus arteriosus | - | Non-differential |
| Transposition of great artery (TGA) | (ASD / VSD) & PDA | Reverse differential |
| Tricuspid atresia | ASD & (VSD / PDA) | Non-differential |
| Tetralogy of Fallot (TOF) | VSD & PDA | Non-differential |
| Total anomalous pulmonary venous return (TAPVR) | ASD / VSD / PDA | Non-differential |
| Hypoplastic left heart syndrome (HLHS) | ASD & PDA | Non-differential |
| Eisenmenger syndrome of ASD | - | Non-differential |
| Eisenmenger syndrome of VSD | - | Non-differential |
| Eisenmenger syndrome of PDA | - | Differential |
PDA-dependent Cyanotic Congenital Heart Defects (CHD)
- Transposition of great artery (TGA)
- Tetralogy of Fallot (TOF)
- Hypoplastic left heart syndrome (HLHS)
- Critical pulmonary stenosis
- Critical aortic stenosis
- Critical coarctation of the aorta (CoA)
Conditions Associated with Heart Defects
| Defect | Conditions |
|---|---|
| Endocardial cushion defects | Down syndrome |
| Atrial septal defect (ASD) | Down syndrome Fetal alcohol syndrome |
| Ventricular septal defect (VSD) | Down syndrome Fetal alcohol syndrome VACTERL association Apert syndrome |
| Patent ductus arteriosus (PDA) | Congenital rubella |
| Tetralogy of Fallot (TOF) | DiGeorge syndrome Velocardiofacial syndrome |
| Mitral valve prolapse (MVP) | Ehlers-Danlos syndrome (EDS) Marfan syndrome Fragile X syndrome Rheumatic fever ADPKD |
| Supravalvular aortic stenosis | Williams syndrome |
| Bicuspid aortic value Coarctation of the aorta (CoA) | Turner syndrome |
| Ebstein anomaly | Lithium |
| Libman-Sacks endocarditis | Systemic lupus erythematosus (SLE) |
| Coronary artery aneurysms | Kawasaki disease |
| Aortic dissection | Ehlers-Danlos syndrome (EDS) Marfan syndrome Tertiary syphilis |
Presentation of Tetralogy of Fallot (TOF) {PROV}
- Pulmonary stenosis
- RV hypertrophy
- Overriding aorta
- Ventricular septal defect
Classification of Heart Failure (HF)
| HFrEF | HFpEF | |
|---|---|---|
| LVEDV | ↑ | ↓ |
| LVESV | ↑ | ↓ |
| SV | ↓ | ↓ |
| LVEF | ↓ | - |
| Dysfunction | Systolic | Diastolic |
| Etiology | ACS & DCMP | HCMP & RCMP |
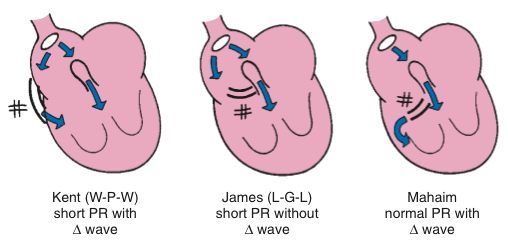
Staging of Heart Failure (HF)
NYHA
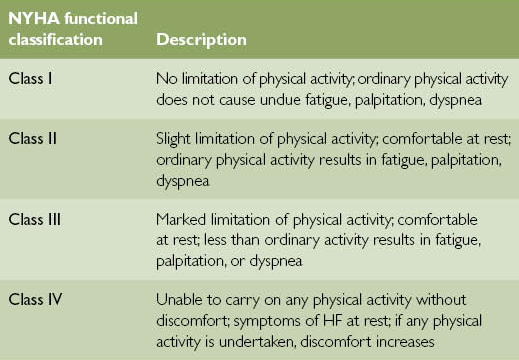
ACC/AHA
Management of Heart Failure (HF)
Decompensated {LMNOP}
- Diuretics :: Lasix
- Venodilators
- Morphine
- Nitrates
- Oxygen
- Position
Compensated {ABVD}
- ACEI & ARB
- β1 antagonists
- Carvedilol
- Bisoprolol
- Metoprolol
- Vasodilators :: Nitrates
- Diuretics :: Spironolactone
- Digitalis
- SGLT-2 inhibitors
- Cardiac resynchronization therapy (CRT)
Indications for CRT in Heart Failure (HF)
- NYHA class II / III / IV
- LV ejection fraction < 35%
- Left bundle branch block (LBBB) w/ QRS complex > 150 ms
Cardiomyopathy
- Dilated cardiomyopathy (DCMP)
- Hypertrophic cardiomyopathy (HCMP)
- Restrictive cardiomyopathy (RCMP)
Etiology of Dilated Cardiomyopathy (DCMP) {ABCD}
- Alcohol
- Beriberi & Vitamin B1 deficiency
- Coxsackie B virus myocarditis
- Cocaine
- Chagas disease
- Doxorubicin
- Duchenne muscular dystrophy (DMD)
Etiology of Arrhythmia {HIS-BEDS}
- Hypoxia
- Ischemia
- Irritability
- Sympathetic tone
- Bradycardia
- Electrolyte disturbances
- Drugs
- Stretch
Pathogenesis of Arrhythmias
- Automaticity
- Triggered activity
- Early after-depolarization (EAD)
- Delayed after-depolarization (DAD)
- Reentry
- Conduction delay
Classification of Arrhythmias
Sinus Arrhythmias
- Sinus bradycardia
- Sinus tachycardia
Supraventricular Arrhythmias :: Atrial
- Atrial tachycardia (AT)
- Focal atrial tachycardia (FAT)
- Multifocal atrial tachycardia (MAT)
- Atrial flutter
- Atrial fibrillation (AF)
Supraventricular Arrhythmias :: Junctional
- Junctional escape [Idiojunctional] rhythm
- Junctional tachycardia (JT)
- AV nodal reentrant tachycardia (AVNRT)
- AV reentrant/reciprocating tachycardia (AVRT)
Ventricular Arrhythmias
- Ventricular escape [Idioventricular] rhythm
- Ventricular tachycardia (VT)
- Ventricular fibrillation (VF)
Types of Pre-excitation
- Wolff-Parkinson-White (WPW) syndrome
- Lown-Ganong-Levine syndrome (LGL) syndrome
Risk of Stroke from Atrial Fibrillation
CHADS2 Score
- Congestive heart failure (CHF)
- Hypertension
- Age ≥ 75 years
- Diabetes mellitus
- Stroke / CVA history
CHA2DS2-VASc Score
- Congestive heart failure (CHF)
- Hypertension
- Age ≥ 75 years
- Diabetes mellitus
- Stroke / CVA history
- Vascular diseases
- Age 65 ~ 75 years
- Sex :: female
Treatment of Atrial Fibrillation
- Cardioversion
- Hemodynamic instability
- Persistence
- Duration < 48 hours
- Anticoagulated
- No atrial thrombus on TEE
- Anticoagulants
- Duration > 48 hours
- CHA2DS2-VASc ≥ 2
- Antiarrhythmics
- Rate control :: Class 2 & 4 & Digitalis
- Rhythm control :: Class 1C & 3
Rules of Malignancy for PVC
- Frequent PVC
- Consecutive PVC
- R-on-T phenomenon
- Acute myocardial infraction
- Multiform PVC
Etiology of QT Prolongation
- Drugs {ABCDE}
- Electrolyte disturbances
- Hypokalemia
- Hypocalcemia
- Hypomagnesemia
- Congenital long QT syndrome
Antiarrhythmics
| Class | Mechanism | Medication |
|---|---|---|
| 1 | Na channel blockers | Class 1A: Quinidine Procainamide Disopyramide |
| Class 1B: Lidocaine Mexiletine | ||
| Class 1C: Flecainide Propafenone | ||
| 2 | β antagonists | - |
| 3 | K channel blockers | Amiodarone Ibutilide Dofetilide Sotalol |
| 4 | Ca channel blockers | Verapamil Diltiazem |
| - | - | Adenosine Digitalis Magnesium |
Effects of Antiarrhythmics on ECG
| ECG | Heart | Phase | Ion Channel | Antiarrhythmics |
|---|---|---|---|---|
| Heart rate | SA node | 4 | Na & K | Class 2 |
| PR interval | AV node | 0 | Ca | Class 2 & 4 |
| QRS complex | Ventricle | 0 | Na | Class 1 |
| QT interval | Ventricle | 2 & 3 | K | Class 1 & 3 |
Contraindications to Amiodarone
- Sinus bradycardia :: < 40/min
- Sick sinus syndrome
- AV blocks
- 2nd degree Mobitz II
- 3rd degree
- Pre-excitation syndrome
- QT prolongation
Indications for Defibrillation
| Condition | Energy (J) |
|---|---|
| VF | 120 ~ 200 |
| Pulseless VT | 120 ~ 200 |
| Unstable polymorphic VT | 120 ~ 200 |
Indications for Synchronized Cardioversion
| Condition | Energy (J) |
|---|---|
| Unstable narrow-QRS tachycardia | 50 ~ 100 |
| Unstable atrial flutter | 50 ~ 100 |
| Unstable atrial fibrillation | 120 ~ 200 |
| Unstable monomorphic VT | > 100 |
Indications for Implantable Cardioverter Defibrillator (ICD)
- History of cardiac arrest due to ventricular arrhythmia w/o reversible cause
- Reduced ejection fraction
- LV ejection fraction < 35% & NYHA class II / III
- LV ejection fraction < 30% & History of MI
Indications for Permanent Pacemaker
- Symptomatic sinus bradycardia :: < 40/min
- Symptomatic sick sinus syndrome
- AV blocks
- 2nd degree Mobitz II
- 3rd degree
Etiology of ST Segment Elevation
- Acute myocardial infarction
- Acute myocarditis
- Acute pericarditis
- Apical ballooning syndrome
- Brugada syndrome
- Hyperkalemia
- Hypothermia
- J point elevation
- Pulmonary embolism
- Variant angina
Coronay Artery Disease (CAD)
| Type | Pathogenesis | T Wave | ST Segment | Q Wave | Triggers | Cardiac Enzymes |
|---|---|---|---|---|---|---|
| Variant [Prinzmetal] angina | Coronary artery spasm | HTW | STE | - | Drugs | - |
| Stable angina | Coronary artery thrombosis | - | STD | - | Exertion | - |
| Unstable angina | Coronary artery thrombosis | TWI | STD | - | Anytime | - |
| NSTEMI | Subendocardial infarction | TWI | STD | - | Anytime | ↑ |
| STEMI | Transmural infarction | HTW | STE | PQW | Anytime | ↑ |
Risk Factors for Coronay Artery Disease (CAD)
- Elderly
- Age ≥ 45 years in males
- Age ≥ 55 years in females
- Family history
- Diabetes
- Hypertension
- HDL < 40 mg/dL
- Cigarette smoking
Diagnosis of STEMI
- ST elevation
- In all leads except V2 and V3: > 1 mm
- In V2 and V3
- In females: > 1.5 mm
- In males age ≥ 40 years: > 2 mm
- In males age < 40 years: > 2.5 mm
- Left bundle branch block (LBBB)
TIMI Risk Score (TRS) for Unstable Angina and NSTEMI {ACS}
- Age > 65 years
- Aspirin use
- Angina ≥ 2 in 24 hours
- CAD history
- CAD risk factors ≥ 3
- Cardiac enzymes
- ST changes > 0.5 mm
| Score | Risk | Management |
|---|---|---|
| < 3 | Low | Cardiac stress test |
| ≥ 3 | High | Coronary angiography |
Management of Acute Coronary Syndrome (ACS)
Acute {MONAB}
- Oxygen
- Venodilators
- Morphine
- Nitrates
- Antiplatelets
- Aspirin
- ADP antagonists
- Gp2b/3a inhibitors
- Anticoagulants :: Heparin
- β1 antagonists
- Revascularization
- Thrombolysis if duration < 12 ~ 24 hours
- Percutaneous intervention (PCI)
- Coronary artery bypass grafting (CABG)
Long-Term
- ACEI & ARB
- Antiplatelets
- β1 antagonists
- Statins
Ideal Door-to-Reperfusion Time for ACS
- Door-to-needle < 30 minutes
- Door-to-bolloon < 90 minutes
Indications for Coronary Artery Bypass Grafting (CABG)
- LCA > 50% stenosis
- Proximal LAD > 50% stenosis
- 2-vessel disease: 2 vessels > 50% stenosis & EF < 50%
- 3-vessel disease: 3 vessels > 50% stenosis
Types of Grafts for Coronary Artery Bypass Grafting (CABG)
- Saphenous vein
- Internal mammary artery (IMA)
- Left internal mammary artery (LIMA)
- Right internal mammary artery (RIMA)
- Radial artery
Complications of Myocardial Infarction
| Time (days) | Histology | Complications |
|---|---|---|
| < 1 | Coagulative necrosis Contraction bank Wavy fiber | Cardiogenic shock Arrhythmia Heaert failure |
| 1 ~ 3 | - | Fibrinous pericarditis |
| 3 ~ 14 | Granulation tissue | Pseudo-aneurysm Free wall rupture Papillary muscle rupture |
| > 14 | Contracted scar | Aneurysm Mural thrombus Dressler syndrome |
Comparison Between Biosprosthetic and Mechanical Heart Valves
| Endpoint | Outcome |
|---|---|
| Mortality | Biosprosthetic > Mechanical |
| Durability | Biosprosthetic < Mechanical |
| Bleeding | Biosprosthetic < Mechanical |
| Thromboembolism | Biosprosthetic < Mechanical |
Beck Triad of Cardiac Tamponade
- Hypotension & Pulsus paradoxus
- Jugular vein distension (JVD) & Kussmaul sign
- Distant heart sound
Pathogens of Infective Endocarditis
- Staphylococcus aureus
- Staphylococcus epidermidis
- Streptococcus viridans
- Enterococcus
- Pseudomonas aeruginosa
- Candida
Pathogens of Culture-Negative Infective Endocarditis {HACEK}
- Haemophilus parainfluenzae
- Actinobacillus
- Cardiobacterium
- Eikenella
- Kingella
Presentation of Infective Endocarditis {FROM-JANE}
- Fever
- Roth spots
- Osler nodes
- Murmur
- Janeway lesions
- Anemia
- Nail-bed hemorrhage
- Emboli
Duke Criteria for Infective Endocarditis
Major
- Microbiological evidence
- Endocardial involvement
Minor
- Fever
- Vascular phenomena
- Immunologic phenomena
- Microbiological evidence
- Risk factors
Empirical Antibiotics for Infective Endocarditis
- Anti-MRSA
- Anti-pseudomonal β-lactams
- ± Aminoglycosides
Management of Pericarditis
| Etiology | Management |
|---|---|
| Bacterial | Antibiotics |
| Viral | NSAIDs Colchicine |
| Fibrinous | Aspirin |
| Uremic | Corticosteroids |
Radiation Heart Disease
- Coronay artery disease (CAD)
- Valvular heart disease
- Aortic regurgitation (AR)
- Aortic stenosis (AS)
- Restrictive cardiomyopathy (RCMP)
- Constrictive pericarditis