Hematolymphoid System
Leukocyte Dysfunctions
| Step | Endothelium | Leukocyte | Disease |
|---|---|---|---|
| Adhesion | CAM | Integrin | Leukocyte adhesion deficiency (LAD) |
| Fusion | - | Microtubule | Chediak-Higashi syndrome (CHS) |
| Degradation | - | NADPH oxidase | Chronic granulomatous disease (CGD) |
| - | Myeloperoxidase | Myeloperoxidase deficiency |
Presentation of Chediak-Higashi Syndrome (CHS)
- Lymphohistiocytosis
- Albinism :: partial
- Recurrent infections
- Neurodegeneration
- Peripheral neuropathy
Immunodeficiency {WASH-CHILD-CBS}
Combined Deficiency {WASH}
| Disease | Gene | Inheritance | IgM | IgG | IgE | IgA |
|---|---|---|---|---|---|---|
| Wiskott-Aldrich syndrome (WAS) | WAS | XR | ↓ | - | ↑ | ↑ |
| Ataxia telangiectasia | ATM | AR | - | ↓ | ↓ | ↓ |
| Severe combined immunodeficiency (SCID) | ADA | AR | ↓ | ↓ | ↓ | ↓ |
| IL-2R | XR | ↓ | ↓ | ↓ | ↓ | |
| Hyper-IgM syndrome | CD40L | XR | ↑ | ↓ | ↓ | ↓ |
T Cell Deficiency {CHILD}
| Disease | Gene | Inheritance | IgM | IgG | IgE | IgA |
|---|---|---|---|---|---|---|
| Chronic mucocutaneous candidiasis | AIRE | AR | - | - | - | - |
| Hyper-IgE [Job] syndrome | STAT3 | AD | - | - | ↑ | - |
| IL-12R deficiency | IL-12R | AR | - | - | - | - |
| DiGeorge syndrome | 22q11 | AD | - | - | - | - |
B Cell Deficiency {CBS}
| Disease | Gene | Inheritance | IgM | IgG | IgE | IgA |
|---|---|---|---|---|---|---|
| Common variable immunodeficiency (CVID) | - | - | ↓ | ↓ | ↓ | ↓ |
| Bruton agammaglobulinemia | BTK | XR | ↓ | ↓ | ↓ | ↓ |
| Selective IgA deficiency | - | - | - | - | - | ↓ |
Presentation of Wiskott-Aldrich syndrome (WAS) {WATER}
- Wiskott
- Aldrich
- Thrombocytopenia
- Eczema ← ↑ IgE & IgA
- Recurrent infections
Presentation of Hyper-IgE [Job] Syndrome {FATE}
- Facies :: coarse
- Abscess
- Teeth :: primary
- Eosinophilia
- Eczema ← ↑ IgE
Gell-Coombs Classification of Hypersensitivity {ACID}
Anaphylactic [Type 1]
| Disease | Antibodies |
|---|---|
| Atopy | IgE |
| Anaphylaxis | IgE |
| Transfusion reaction :: allergic | IgE |
| Urticaria | IgE |
Cytotoxic [Type 2]
| Disease | Antibodies |
|---|---|
| Autoimmune hemolytic anemia (AHA) | Anti-RBC |
| Bullous pemphigoid | Anti-hemidesmosome |
| Goodpasture syndrome | Anti-basement membrane |
| Graves disease | Anti-TSH receptor |
| Guillain-Barre syndrome | Anti-ganglioside |
| Heparin-induced thrombocytopenia (HIT) | Anti-platelet factor 4 (Anti-PF4) |
| Immune thrombocytopenic purpura (ITP) | Anti-Gp1b Anti-Gp2b/3a |
| Lambert-Eaton myasthenic syndrome | Anti-presynatic Ca channel |
| Membranous nephropathy | Anti-phospholipase A2 receptor (Anti-PLA2R) |
| Myasthenia gravis | Anti-ACh receptor |
| Pemphigus vulgaris | Anti-desmosome |
| Pernicious anemia | Anti-parietal cell Anti-intrinsic factor |
| Rheumatic fever | Anti-M protein |
| Transfusion reaction :: hemolytic | Anti-ABO Anti-Rh |
| Transfusion reaction :: febrile non-hemolytic | Anti-WBC |
| Transplant reaction :: hyperacute | Anti-graft |
Immune Complex-Mediated [Type 3]
| Disease | Antibodies |
|---|---|
| ANCA-associated vasculitis (AAV) | Anti-PR3 [c-ANCA] Anti-MPO [p-ANCA] |
| Antiphospholipid syndrome (APS) | Anti-cardiolipin Anti-β2-glycoprotein I Lupus anticoagulant |
| Arthus reaction | - |
| Autoimmune hepatitis | Anti-smooth muscle Anti-Liver kidney microsomal (Anti-LKM) Anti-liver cytosol (Anti-LC) |
| Crohn disease | ASCA |
| Dermatitis herpetiformis | Anti-tissue transglutaminase (Anti-tTG) IgA |
| Drug-induced lupus | Anti-histone |
| IgA nephropathy [Berger disease] | IgA |
| IgA vasculitis [Henoch-Schonlein purpura (HSP)] | IgA |
| Membranoproliferative glomerulonephritis (MPGN) | C3 nephritic factor |
| Mixed connective tissue disease (MCTD) | Anti-U1 RNP |
| Polyarteritis nodosa | - |
| Polymyositis Dermatomyositis | Anti-Jo-1 Anti-Mi-2 Anti-SRP |
| Primary biliary cirrhosis (PBC) | Anti-mitochondrium |
| Primary sclerosing cholangitis (PSC) | Anti-MPO [p-ANCA] |
| Rheumatoid arthritis | Rheumatoid factor [Anti-IgG] Anti-CCP |
| Scleroderma :: diffuse | Anti-Scl-70 [Anti-topoisomerase] |
| Scleroderma :: limited | Anti-centromere |
| Serum sickness | - |
| Sjogren syndrome | Anti-Ro [Anti-SSA] Anti-La [Anti-SSB] |
| Systemic lupus erythematosus (SLE) | Anti-dsDNA Anti-Smith [Anti-snRNP] |
| Ulcerative colitis | Anti-MPO [p-ANCA] |
Delayed [Type 4]
| Disease | Antibodies |
|---|---|
| Celiac disease | Anti-tissue transglutaminase (Anti-tTG) IgA Anti-endomysial IgA Anti-gliadin IgA |
| Contact dermatitis | - |
| DM type 1 | Anti-glutamate decarboxylase (Anti-GAD-65) |
| Graft-versus-host disease (GVHD) | - |
| Hashimoto thyroiditis | Anti-thyroglobulin Anti-TPO Anti-microsome |
| Multiple sclerosis | - |
| Tuberculin skin test (TST) | - |
| Stevens-Johnson syndrome (SJS) | - |
| Toxic epidermal necrolysis (TEN) | - |
| Transplant reaction :: acute | - |
| Transplant reaction :: chronic | - |
Presentation of Atopy
- Allergic conjunctivitis
- Allergic rhinitis
- Asthma
- Atopic dermatitis
Diagnostic Criteria for Anaphylaxis
- Hypotension
- Respiratory compromise
- Skin mucosal tissue symptoms
- Gastrointestinal symptoms
HLA Subtypes Associated With Diseases
| HLA | Diseases |
|---|---|
| A3 | Hemochromatosis |
| B27 | Psoriatic arthritis Ankylosing spondylitis Inammatory bowel disease Reactive arthritis |
| B51 | Behcet disease |
| B5801 | Stevens-Johnson syndrome (SJS) |
| DQ2 DQ8 | Celiac disease |
| DR2 | Multiple sclerosis Hay fever SLE Goodpasture syndrome |
| DR3 | DM type 1 SLE Graves disease Hashimoto thyroiditis |
| DR4 | Rheumatoid arthritis DM type 1 |
| DR5 | Pernicious anemia Hashimoto thyroiditis |
Etiology of Cold Sensitive Antibodies (CSA)
- Infection
- Mycoplasma
- HCV
- EBV
- Autoimmune disorders
- IgM monoclonal gammopathy
- Waldenstrom macroglobulinemia
- IgM monoclonal gammopathy of undetermined significance (MGUS)
Jones Criteria for Rheumatic Fever {JONES}
- Joint :: migratory polyarthritis
- Heart :: mitral regurgitation & stenosis
- Nodules :: subcutaneous
- Erythema marginatum
- Sydenham chorea [Chorea minor]
Presentation of Sarcoidosis {GAUSH}
- Granuloma :: non-caseating
- γ globulinemia
- ↑ Angiotensin converting enzyme (ACE)
- Asteroid body
- Arthritis
- Uveitis
- Schaumann body
- ↑ 1α-hydroxylase
- Hypercalcemia
Triad of Lofgren Syndrome
- Erythema nodosum
- Adenopathy :: hilar
- Arthritis :: migratory
Seronegative Spondyloarthropathy {PAIR}
- Psoriatic arthritis
- Ankylosing spondylitis
- Inflammatory bowel disease
- Reactive arthritis [Reiter syndrome]
Precipitating Factors of Reactive Arthritis
- Chlamydia
- Campylobacter
- Salmonella
- Shigella
- Ureaplasma
Triad of Reactive Arthritis {AUC}
- Arthritis
- Urethritis
- Conjunctivitis
SLICC Diagnostic Criteria for SLE {MD-SOAP-BRAIN}
- Malar rash
- Discoid rash
- Serositis
- Oral ulcer
- Arthritis
- Photosensitivity
- Blood disorders
- Renal disorders
- Autoimmune antibody
- Immunologic disorders
- Neurologic disorders
Presentation of Rheumatoid Arthritis
- Pannus
- Symmetric polyarthritis
- Swan neck deformity
- Boutonniere deformity
- Ulnar deviation
- Atlanto-axial subluxation
- Keratoconjunctivitis sicca
Diagnostic Criteria for Rheumatoid Arthritis
- Polyarthritis :: joints ≥ 3
- Chronicity :: duration > 6 weeks
- Positive RF / Anti-CCP
- Elevated ESR / CRP
- Exclusion of alternative diagnoses
Disorders Associated with Rheumatoid Arthritis
Felty syndrome
- Rheumatoid arthritis
- Splenomegaly
- Neutropenia
Caplan syndrome
- Rheumatoid arthritis
- Pneumoconiosis
- Lung nodules
Treatment of Rheumatoid Arthritis
| Mechanism | Medication |
|---|---|
| COX inhibitors | NSAIDs |
| Sulfasalazine Mesalazine | |
| ↓ Folate synthesis | Methotrexate |
| ↓ Purine synthesis | Azathioprine |
| ↓ Pyrimidine synthesis | Leflunomide |
| ↑ DNA crosslinking | Cyclophosphamide |
| NF-κB inhibitors | Corticosteroids |
| TNF-α inhibitors | Infliximab Adalimumab |
| CD20 inhibitors | Rituximab |
| - | Chloroquine |
Presentation of Limited Scleroderma {CREST}
- Calcinosis
- Raynaud syndrome
- Esophageal dysmotility
- Sclerodactyly
- Telangiectasia
Triad of Henoch-Schonlein Purpura (HSP)
- Abdominal pain
- Arthritis
- Rashes
- ± IgA nephropathy [Berger disease]
Presentation of Dermatomyositis
- Heliotrope sign
- Shawl sign
- Gottron sign
- Gower sign
- Proximal muscle weakness
Diagnostic Criteria for Antiphospholipid Syndrome (APS)
- Clinical criteria ≥ 1
- Vascular thrombosis
- Pregnancy morbidity
- Unexplained fetal death > 10 weeks of gestation
- Premature births of due to eclampsia / placental insufficiency
- Three unexplained consecutive spontaneous abortions < 10 weeks of gestation
- Laboratory criteria ≥ 1
- Lupus anticoagulant at least twice > 12 weeks apart
- Anti-cardiolipin at least twice > 12 weeks apart
- Anti-β2 glycoprotein at least twice > 12 weeks apart
Presentation of Adult-onset Still's Disease
- Arthralgia
- Fever
- ↑ Ferritin
- Hepatomegaly
- Leukocytosis
- Lymphadenopathy
- Rashes :: salmon-colored
- Splenomegaly
Types of Transplants
- Autograft
- Isograft
- Allograft
- Xenograft
Types of Transplant Reactions
| Type | Causes | Onset |
|---|---|---|
| Hyperacute | Anti-graft | Minutes |
| Acute | T-cell | Days ~ Weeks |
| Chronic | T-cell | Months ~ Years |
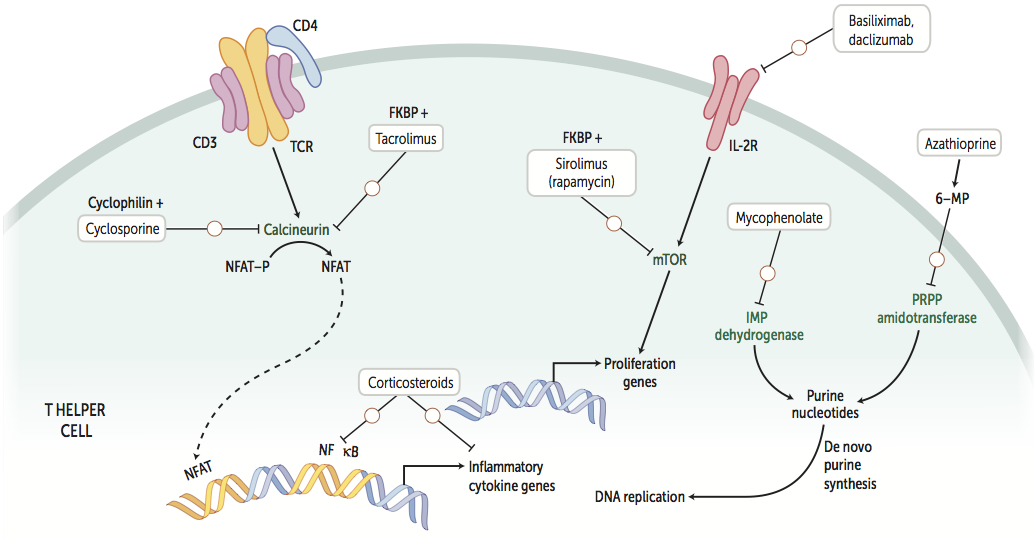
Immunosuppressants
| Mechanism | Medication | Indications |
|---|---|---|
| COX inhibitors | NSAIDs | Immunosuppression |
| ↓ Folate synthesis | Methotrexate | Immunosuppression |
| ↓ Purine synthesis | Mycophenolate Azathioprine | Immunosuppression |
| ↓ Pyrimidine synthesis | Leflunomide | Immunosuppression |
| ↑ DNA crosslinking | Cyclophosphamide | Immunosuppression |
| NF-κB inhibitors | Corticosteroids Mesalazine | Immunosuppression |
| Calcineurin inhibitors | Cyclosporine Tacrolimus | Immunosuppression |
| mTOR inhibitors | Sirolimus Everolimus | Immunosuppression |
| IL-2R inhibitors | Basiliximab Daclizumab | Immunosuppression |
| TNF-α inhibitors | Etanercept | Immunosuppression |
| Infliximab Adalimumab | Immunosuppression | |
| CD20 inhibitors | Rituximab | Immunosuppression |
Etiology of Target Cells {HALT}
- HbC disease
- Asplenia
- Liver disease
- Thalassemia
Etiology of Anemia
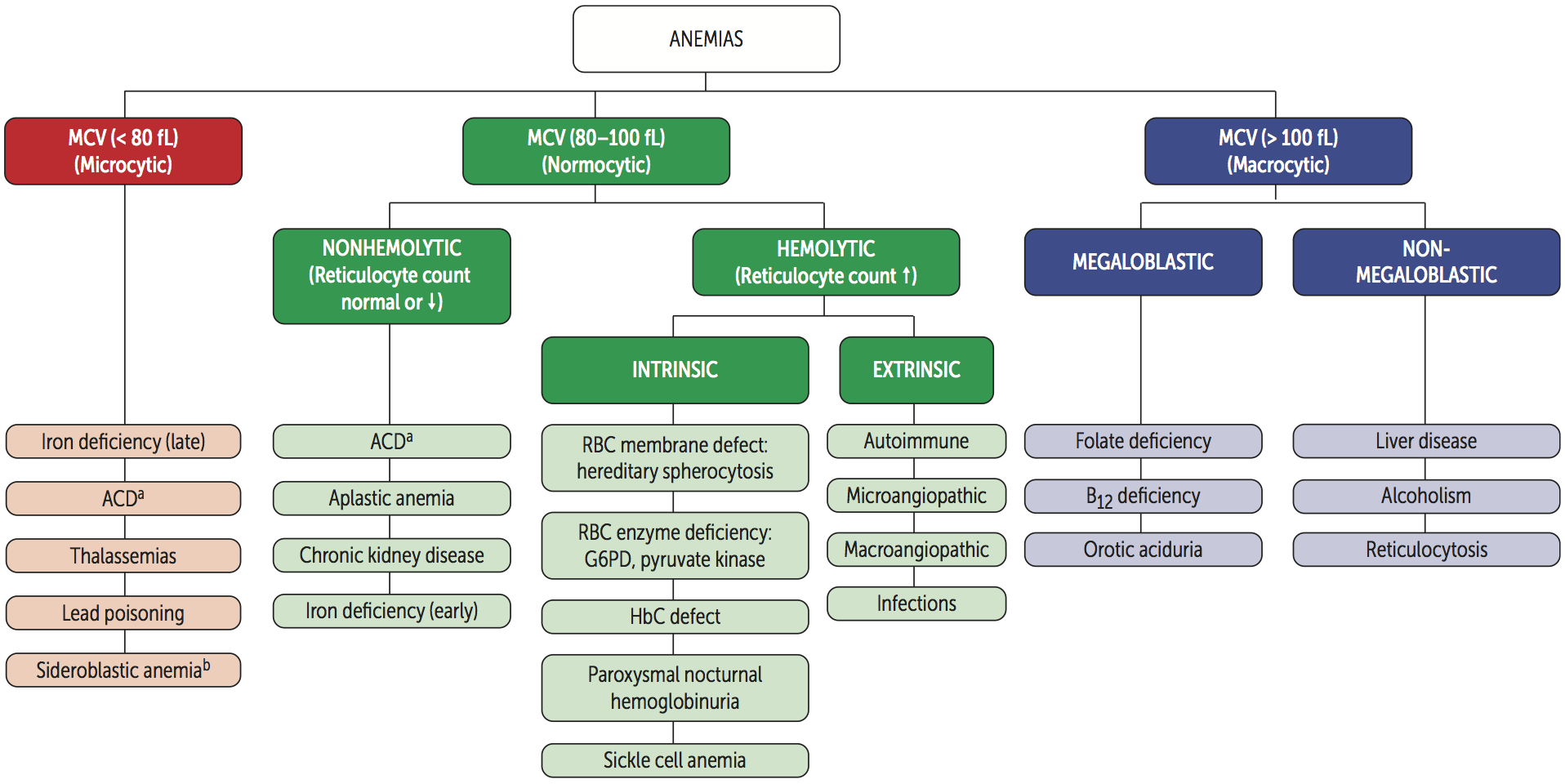
Microcytic Anemia {TAILS}
| Anemia | Fe | Ferritin | Transferrin [TIBC] | Saturation = Fe ÷ TIBC | Defect |
|---|---|---|---|---|---|
| Thalassemia | - | - | - | - | Hemoglobin |
| Anemia of chronic disease (ACD) | ↓ | ↑ | ↓ | - | Fe |
| Iron deficiency anemia (IDA) | ↓ | ↓ | ↑ | ↓ | Fe |
| Lead poisoning | ↑ | ↑ | ↓ | ↑ | Heme |
| Sideroblastic anemia | ↑ | ↑ | ↓ | ↑ | Heme |
Normocytic Anemia
Non-hemolytic Anemia
- Aplastic anemia
- Chronic kidney disease (CKD)
Hemolytic Anemia
| Intravascular | Extravascular | |
|---|---|---|
| Peripheral smear | Schistocyte | Spherocyte |
| Haptoglobin | ↓ | - |
| Hemoglobin | ↑ | - |
| Hematuria | + | - |
| Indirect bilirubin | - | ↑ |
| Direct bilirubin | - | - |
| Urine bilirubin | - | - |
| Urine urobilinogen | - | ↑ |
| LDH | ↑ | ↑ |
| Jaundice | - | + |
Intravascular Hemolytic Anemia {TIMP}
- Transfusion
- Infusion
- Macroangiopathic hemolytic anemia (MAHA)
- Microangiopathic hemolytic anemia (MAHA)
- Disseminated intravascular coagulation (DIC)
- Thrombotic thrombocytopenic purpura (TTP)
- Hemolytic uremic syndrome (HUS)
- HELLP syndrome
- Paroxysmal nocturnal hematuria (PNH)
Extravascular Hemolytic Anemia {PHAGES}
- Pyruvate kinase deficiency
- HbC disease
- Hereditary spherocytosis
- Autoimmune hemolytic anemia (AHA)
- G6PD deficiency
- Elliptocytosis
- Sickle cell disease (SCD)
Macrocytic Anemia
Megaloblastic
- Folate deficiency
- Vitamin B12 deficiency
- Orotic aciduria
- Fanconi anemia
Non-megaloblastic
- Diamond-Blackfan anemia
- Alcoholism
- Reticulocytosis
Etiology of Elevated RDW
- Iron deficiency anemia (IDA)
- Folate deficiency anemia
- Vitamin B12 deficiency anemia
- Mixed anemia
Comparison Between Thalassemia and IDA
| Thalassemia | IDA | |
|---|---|---|
| Mentzer index = MCV ÷ RBC | < 13 | > 13 |
| RDW | - | ↑ |
| Iron profile | Normal | Abnormal |
| Blood smear | Target cells | - |
Etiology of Aplastic Anemia
- Fanconi anemia
- Virus
- Parvovirus B19
- EBV
- CMV
- HIV
- Hepatitis virus
- Drugs
- Carbamazepine
- Methimazole
- Propylthiouracil
- NSAIDs
- Chloramphenicol
- Toxins :: Benzene
- Radiation
Presentation of Sickle Cell Disease (SCD)
- Vaso-occlusive crisis (VOC)
- Acute chest syndrome
- Mesenteric ischemia
- Ischemic stroke
- Hemolysis :: extravascular
- Splenic sequestration
- Aplastic crisis
- Avascular necrosis
- Osteomyelitis
- Dactylitis
- Priapism
Triggers of Vaso-occlusive Crisis (VOC) in Sickle Cell Disease (SCD)
- Dehydration
- Infection
- Hypoxia
- Cold temperatures
Management of Sickle Cell Disease (SCD)
- Immunizations
- Penicillin prophylaxis
- Folate supplementation
- Transfusion
- Hemapheresis
- Hydroxyurea
- Bone marrow transplantation
Treatment of Polycythemia
- Phlebotomy
- Antiplatelets :: Aspirin
- Cytoreductive agents
- Hydroxyurea
- Interferon
- Busulfan
Abnormal Hemoglobin Variants
| α-Globin | Disease | α-Globin Defect | Disease | |
|---|---|---|---|---|
| β-Globin | α2β2 [HbA] | - | β4 [HbH] | α-thalassemia :: 3 deletion |
| γ-Globin | α2γ2 [HbF] | β-thalassemia major | γ4 [Hb Barts] | α-thalassemia :: 4 deletion |
| δ-Globin | α2δ2 [HbA2] | β-thalassemia minor | - | - |
| s-Globin | α2s2 [HbS] | Sickle cell disease | - | - |
| c-Globin | α2c2 [HbC] | HbC disease | - | - |
Heme Synthesis Disorders
- Lead poisoning
- Sideroblastic anemia
- Alcoholism
- ALA synthase deficiency
- Vitamin B6 deficiency
- Copper deficiency
- Porphyria
Types of Porphyria
- Acute intermittent porphyria (AIP)
- Porphyria cutanea tarda (PCT)
- Erythropoietic protoporphyria (EPP)
Presentation of Acute Intermittent Porphyria (AIP) {5P}
- Pain :: abdomen
- Port wine-colored urine
- Peripheral neuropathy
- Psychological disturbances
- Precipitation
- Starvation
- Alcohol
- Cytochrome P-450 (CYP450) inducers
Types of Transfusion Reactions
| Type | Causes | Onset |
|---|---|---|
| Allergic | Anti-plasma proteins IgE Anti-IgA IgE | Minutes ~ Hours |
| Hemolytic (HTR) | Anti-ABO Anti-Rh | Minutes ~ Days |
| Febrile non-hemolytic (FNHTR) | Anti-WBC | Hours |
Classificaiton of Myeloid Neoplasms
Acute Myelogenous Leukemia (AML)
- AML with defining genetic abnormalities
- AML with myelodysplasia-related changes (AML-MRC)
- Therapy-related AML (t-AML)
- AML, not otherwise specified (NOS)
- M0: Minimally differentiated
- M1: Without maturation
- M2: With maturation
- M3: Acute promyelocytic leukemia (now classified by its genetic marker)
- M4: Acute myelomonocytic leukemia
- M5: Acute monocytic leukemia
- M6: Acute erythroid leukemia
- M7: Acute megakaryoblastic leukemia
Myelodysplastic Syndromes/Neoplasms (MDS)
- Myelodysplastic neoplasms with defining genetic abnormalities
- Myelodysplastic neoplasms, morphologically defined
Myeloproliferative Neoplasms (MPN)
| Tumors | Genetics | RBC | WBC | PLT |
|---|---|---|---|---|
| Polycythemia vera | JAK2 | ↑ | ↑ | ↑ |
| Chronic myelogenous leukemia (CML) | t(9;22) | ↓ | ↑ | ↑ |
| Essential thrombocytosis | JAK2 | - | - | ↑ |
| Myelofibrosis | JAK2 | ↓ | ↑/↓ | ↑/↓ |
Classificaiton of Lymphoid Neoplasms
T-cell Neoplasms
| Tumor | Mutation | Gene |
|---|---|---|
| Adult T-cell lymphoma | - | - |
| Cutaneous T-cell lymphoma | - | - |
B-cell Neoplasms
| Tumor | Mutation | Gene |
|---|---|---|
| Hodgkin lymphoma | - | - |
| Burkitt lymphoma | t(8;14) | C-MYC |
| Diffuse large B-cell lymphoma (DLBCL) | - | - |
| Mantle cell lymphoma | t(11;14) | Cyclin D (CCND) |
| Marginal zone lymphoma MALT lymphoma (MALToma) | - | - |
| Follicular lymphoma | t(14;18) | BCL2 |
Workup of Leukemia
- Peripheral blood smear
- Bone marrow smear
- Cytochemistry
- Immunophenotyping
- Karyotyping
- Genotyping
B Symptoms of Lymphoma
- Fever
- Night sweats
- Weight loss
Treatment of Hodgkin Lymphoma {ABVD}
- Doxorubicin [Adriamycin]
- Bleomycin
- Vinblastine
- Dacarbazine
Treatment of B-cell Non-Hodgkin Lymphoma {R-CHOP}
- Rituximab
- Cyclophosphamide
- Doxorubicin [Hydroxydaunorubicin]
- Vincristine [Oncovin]
- Prednisolone
Causes of Monoclonal Spike [M Spike]
- Multiple myeloma
- Waldenstrom macroglobulinemia
- Monoclonal gammopathy of undetermined significance (MGUS)
- AL amyloidosis
Presentation of Multiple Myeloma {CRAB}
- Hypercalcemia
- Renal failure
- Rouleaux formation
- Russell body
- Anemia
- Amyloidosis :: primary
- Back pain
- Bone lesions
- Bence-Jones protein
Diagnostic Tests for Multiple Myeloma
- Protein electrophoresis
- Bone marrow biopsy
- Skeletal survey
Diagnosis of Multiple Myeloma
- Histology of bone marrow
- Clonal bone marrow plasma cells > 10%
- Plasmacytoma
- Evidence of end-organ damages {CRAB}
- Hypercalcemia
- Renal failure
- Anemia
- Bone lesions
- Evidence of inevitable end-organ damages
- Free light chain (FLC) ratio > 100
- Clonal bone marrow plasma cell > 60%
- Bone lesions on MRI > 1
Presentation of Hemophagocytic Lymphohisticytosis (HLH)
- Fever
- ↑ Ferritin
- Hypertriglyceridemia
- Hemophagocytosis
- ↓ NK cell activity
- Pancytopenia
- Rashes
- Splenomegaly
Virchow Triad for Thrombosis {SHE}
| Cause | Effect |
|---|---|
| Stasis | VTE |
| Hypercoagulability | ATE / VTE |
| Endothelial injury | ATE |
Etiology of Hypocoagulability
| Etiology | Mechanism | PLT | BT | PT | PTT | Clots |
|---|---|---|---|---|---|---|
| Disseminated intravascular coagulation (DIC) | - | ↓ | ↑ | ↑ | ↑ | + |
| Thrombotic thrombocytopenic purpura (TTP) | ↓ ADAMTS13 | ↓ | ↑ | - | - | + |
| Hemolytic uremic syndrome (HUS) | ↓ ADAMTS13 Shiga-like toxin | ↓ | ↑ | - | - | + |
| HELLP syndrome | - | ↓ | ↑ | - | - | - |
| Immune thrombocytopenic purpura (ITP) | Anti-Gp1b Anti-Gp2b/3a | ↓ | ↑ | - | - | - |
| Heparin-induced thrombocytopenia (HIT) | Anti-platelet factor 4 (Anti-PF4) | ↓ | ↑ | - | - | + |
| Antiphospholipid syndrome (APS) | Anti-cardiolipin Anti-β2-glycoprotein I Lupus anticoagulant | - | - | - | ↑ | + |
| Von Willebrand disease (VWD) | ↓ vWF | - | ↑ | - | ↑ | - |
| Bernard-Soulier disease (BSD) | ↓ Gp1b | - | ↑ | - | - | - |
| Glanzmann disease | ↓ Gp2b/3a | - | ↑ | - | - | - |
| Hemophilia A & B & C | ↓ Factor 8 & 9 & 11 | - | - | - | ↑ | - |
| Vitamin K deficiency | ↓ Factor 2 & 7 & 9 & 10 | - | - | ↑ | ↑ | - |
| Cirrhosis | ↓ Thrombopoietin (TPO) ↓ Factors | ↓ | ↑ | ↑ | - | - |
Etiology of Hypercoagulability
| Etiology | Mechanism |
|---|---|
| Homocysteinemia | ↑ Factor 7 |
| Factor 5 Leiden mutation | ↑ Factor 5 |
| Prothrombin gene mutation | ↑ Factor 2 |
| Antithrombin deficiency | ↓ Antithrombin |
| Protein C/S deficiency | ↓ Protein C/S |
| Nephrosis | ↓ Protein C/S |
| Pregnancy | ↑ Factor 1 |
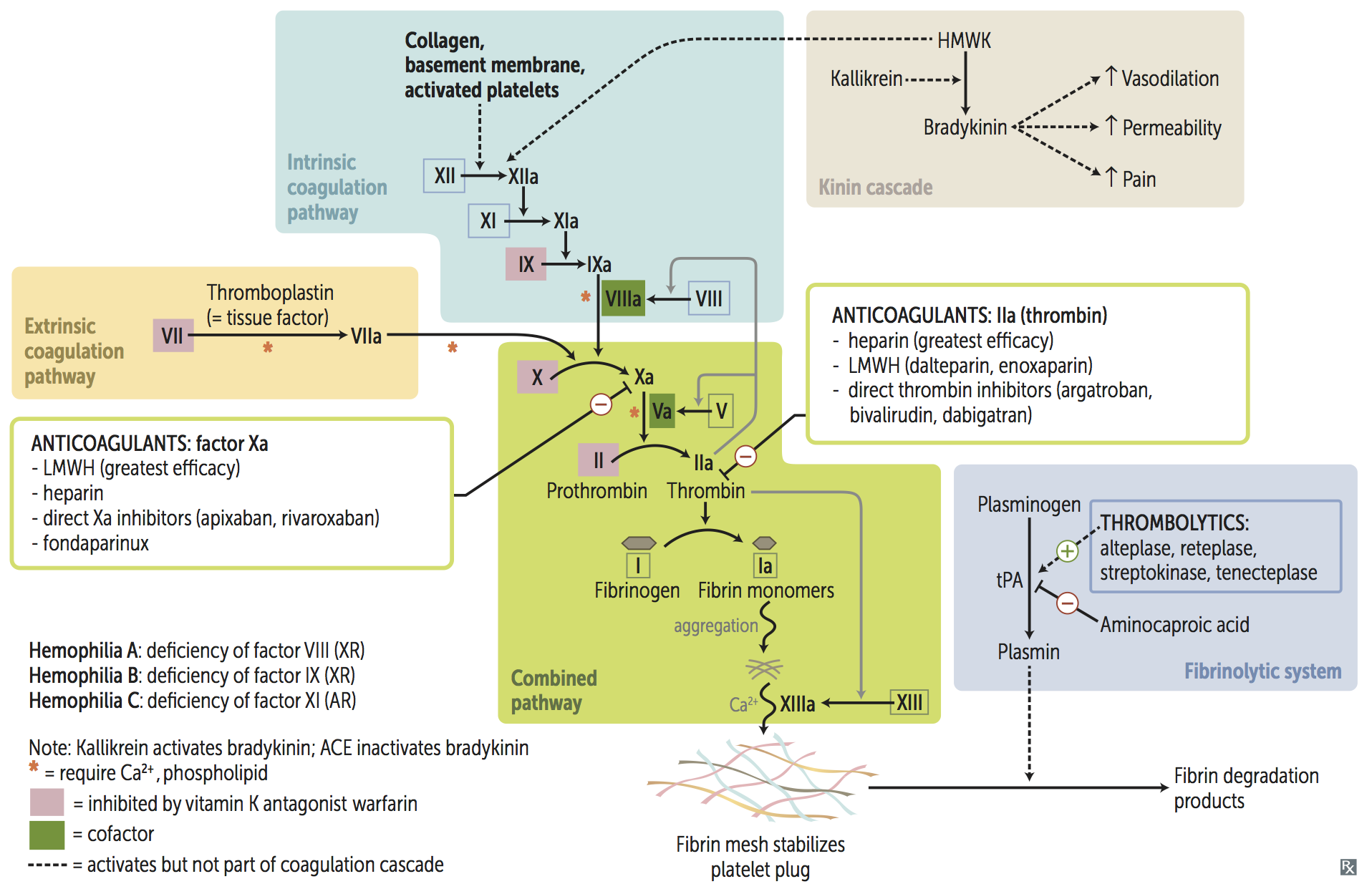
Antiplatelets
| Mechanism | Medication |
|---|---|
| Gp2b/3a inhibitors | Abciximab Eptifibatide Tirofiban |
| ADP antagonists | Clopidogrel Prasugrel Ticagrelor Ticlopidine |
| PDE inhibitors | Dipyridamole Cilostazol |
| COX inhibitors | NSAIDs |
Anticoagulants
| Mechanism | Medication |
|---|---|
| VKOR inhibitors | Warfarin Coumadin |
| Antithrombin inducers | Unfractionated heparin (UFH) |
| Low-molecular-weight heparin (LMWH): Enoxaparin Dalteparin | |
| Fondaparinux | |
| Factor 10a inhibitors | Apixaban Edoxaban Rivaroxaban |
| Factor 2a inhibitors | Hirudin Bivalirudin Argatroban Dabigatran |
| Tissue plasminogen activators (tPAs) | Urokinase Streptokinase Alteplase Reteplase Tenecteplase |
Heparin Variants
| UFH | LMWH | |
|---|---|---|
| Bioavailability | - | ↑ |
| Half-life | - | ↑ |
| Specificity to Factor 10a | - | ↑ |
| Monitor | PTT | - |
| Side Effect | HIT & Osteoporosis | - |
| Antidote | Protamine sulfate | - |
Goal INR
| Condition | INR |
|---|---|
| Venous thromboembolism (VTE) | 2.0 ~ 3.0 |
| Atrial fibrillation | 2.0 ~ 3.0 |
| Bioprosthetic valve | 2.0 ~ 3.0 |
| Mechanical valve | 2.5 ~ 3.5 |
Management of Supratherapeutic INR
| INR | Management |
|---|---|
| < 4.5 | Hold warfarin |
| 4.5 ~ 10 | Hold warfarin Low-dose oral vitamin K |
| > 10 | Hold warfarin High-dose oral vitamin K |
| Bleeding | Hold warfarin High-dose IV viatamin K FFP / PCC |
Etiology of Disseminated Intravascular Coagulation (DIC)
| Mnemonic | Cause |
|---|---|
| S | Sepsis :: GNB |
| T | Trauma |
| O | Obstetric complications |
| P | Pancreatitis :: acute |
| Making | Malignancy |
| New | Nephrotic symdrome |
| Thrombi | Transfusion |
Pentad of Thrombotic Thrombocytopenic Purpura (TTP)
- Renal symptoms
- Anemia
- Thrombocytopenia
- Neurologic symptoms
- Fever
Treatment of Thrombotic Thrombocytopenic Purpura (TTP)
- Plasmapheresis
- Immunosuppression
- Corticosteroids
- Rituximab
Triad of Hemolytic Uremic Syndrome (HUS)
- Renal symptoms
- Anemia
- Thrombocytopenia
Treatment of Immune Thrombocytopenic Purpura (ITP)
- Immunosuppression
- Corticosteroids
- Rituximab
- Intravenous immunoglobulin (IVIG)
- Splenectomy
Indications for Thrombolytics
- ST-elevation myocardial infarction (STEMI)
- Duration < 12 ~ 24 hours
- Door-to-bolloon > 2 hours
- Ischemic stroke
- Duration < 3 ~ 4.5 hours
- BP < 185/110 mmHg
- Pulmonary embolism (PE)
- Hemodynamic instability
Contraindications to Thrombolytics
- Intracranial hemorrhage
- Internal bleeding
- Bleeding tendency
Plasma Products
- Fresh frozen plasma (FFP)
- Prothrombin complex concentrate (PCC)
- Cryoprecipitate
- Factor concentrate
Indications for Plasma Products
| Product | Indications |
|---|---|
| FFP / PCC | Warfarin toxicity Factor 10a inhibitors toxicity |
| Cryoprecipitate | tPA toxicity Fibrinogen deficiency Hemophilia A Von Willebrand disease (VWD) Uremic bleeding |
| Factor concentrate | Factor deficiency |
Antifibrinolytics
- Tranexamic acid
- Aminocaproic acid